|
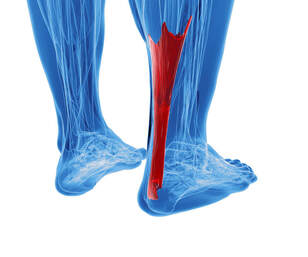
Tricia Hayton, Registered Physiotherapist Since Durant’s recent quick exit from the NBA series, calf injuries have been a hot topic of conversation. What was the initial injury? How did it change so drastically? First, a little anatomy lesson is needed to understand what happened. The calf is made up of two or three muscles. The deepest is a very small muscle called the plantaris. About 20% to 30% of the population do not even have this muscle, however they do not have any change in function or athletic ability. More critical to function, are the soleus and gastrocnemius. These muscles are large, powerful muscles that propel the body up (as in jumping) and forward (as in running). They blend together to form a strong tendon called the Achilles tendon. The initial injury was called a calf strain. This is a small tear or fray of the muscle of the calf. Although technically it can occur anywhere in the gastrocsoleus complex, it most commonly occurs where the head of the gastrocnemius gradually blends into a tendon. If you were to look at a muscular calf, the surface muscle, the gastric, is made up of two circular heads that come together about two-thirds of the way down the shin bone. Where these circular heads come together is where the tendon starts. This is the most common location for a strain. Medically, we grade strains as first, second, or third. A first-degree strain is when the muscle pulls and stretches beyond what is comfortable, but there is no tear of the fibers. A second-degree strain is where the stretch tears some of the muscle fibers, but the muscle is still securely connected to the bones at each end. A third-degree tear is when the muscle tears in two. The injury suffered by Durant during the finals was an Achilles tear or rupture. This is very similar to a Grade three strain. The tendon has been torn in two and is no longer connecting the two bones. This means that the muscle is no longer able to generate any power. Thus, Durant can no longer run or jump. Surgery or serial casting is needed to repair this injury. Each case is analyzed by an orthopedic surgeon and the most appropriate way of completing the repair is decided. Factors considered include age, athletic demands, time span until return to sport, and severity of tear. Complete rehabilitation of this injury typically takes 6 months to return to sport, although we all know that a professional player may bend this rule slightly. I think the critical lesson for those of us in sports medicine is that we need to make sure that we are not encouraging our athletes to return to sport too early. Proper strengthening and healing is critical because although the risk of reinjury may be small, the consequence is huge.
0 Comments
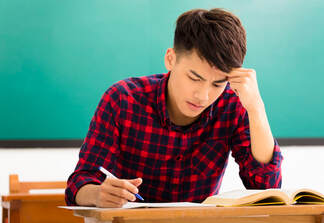
Tricia Hayton, Registered Physiotherapist Concussion is a hot topic in schools. Thousands of students from Kindergarten to university suffer concussions each year. This can be from a fall, a car accident or from sports. Following a concussion, cognitive and physical rest is prescribed. Recent studies have shown us that this rest should be limited to approximately 24 to 48 hours. After that amount of time, sub-symptomatic activities can actually be beneficial in restoring brain function and reducing symptoms. We often hear about athletes returning to sports. Our professional athletes will have “red jersey” practices where they get back to their technical and fitness skills but refrain from contact. When tolerated, they begin contact and eventually return to the games they love. But how does a student return to school? What are the steps? There are some simple guidelines: 1. For student athletes, return to school should precede any attempt to return to sport 2. Like return to sport, return to learn should be coordinated by a trained medical professional. Ideally, a team of professionals including therapists and doctors is best. 3. There are four stages to return to learn. A student progresses through each stage when the current demand is met without any increase in symptoms for a minimum of 24 hours. 4. If symptoms increase as they progress, they are to return to the previous level for a minimum of 24 hours. The stages of return to learn include:
1. Light cognitive activity: this includes reading and games done at home 2. School type work/light physical activity: this is work done that is similar to the demands of school, but in 30-minute blocks. Some light activity, such as going for a walk, is encouraged. 3. Part time school: this can be divided into light load and moderate load, indicating the time spent in school, including hours per day or days per week 4. Nearly normal workload progressing to full time demands: Time and homework are increased as tolerated. At this point, accommodations are often needed as only certain aspects will increase symptoms (ie: reduced computer time). Physical Education class is not included as it should be increased during the return to sport phase. For more information please visit: http://horizon.parachutecanada.org/wp-content/uploads/2017/06/RTL-Parachute-2018May.pdf. The staff at Physio Sport Med work as a team to help guide you through these challenges. If you think that we could help you or someone you love, please give us a call. Tricia Hayton, Registered Physiotherapist Habits of musicians are often compared to elite athletes. They practice for hours a day to perfect their skills to achieve success in a very competitive environment. Like the athlete, these habits can cause damage to the body and result in injury. Injuries that mean time away from gigs, income, and in the worst-case scenario, a change of career. So, what can be done? There are two main factors that contribute to overuse injuries in musicians. 1. Repetition: As it sounds, this means that the body is performing an act over and over again until it is perfected. However, damage begins when there is not adequate rest. Initially, the musician will complain of fatigue and tension near the end of the session. This develops into pain during the session, and then lingering pain when one is away from their instrument. The most common overuse injury is tendonitis. 2. Asymmetry: This refers to the need to hold the body in an unbalanced position for an extended period. An example is a violinist tilting their head to support the instrument as they play. This can alter the movement patterns of a joint, increasing the risk of injury. For example, our violinist may develop a nerve impingement on the side towards her violin due to neck posture and reduced space for the nerves to travel from the neck to the arm.  What are the warning signs? 1. Fatigue near the end of a practice session. This can also be felt as tension at the end, or in between sessions. 2. Tingling in the hand or arm. There are some overuse injuries that can cause neural compression (thoracic outlet syndrome, for example). This compression will often begin with a tingling in the hand and arm that is relieved with a change of position. 3. Weakness of the hand or the feeling of being uncoordinated. 4. Fatigue or discomfort when carrying instrument from a gig or practice. What can be done?
1. Movement Screen: A physiotherapist or sports chiropractor can complete a movement screen. This will give indications where muscle imbalances are building. Exercises will then be given to correct the imbalance (to go back to my athlete comparison – this is the same as cross training). 2. Postural education and core strengthening. 3. Pain management: sometimes you just need to get through a busy time – whether it is a testing period, recital, or short running performance, then you will take rest and let the body heal. Pain management with modalities, acupuncture, or manual therapy can help through this time. Please realize this is not a long-term solution. 4. Technique analysis: looking at your movement screens together with a musical teacher or coach, the method that you use to hold or manipulate the instrument can be slightly altered. Like athletes, musicians may be nervous that this will alter performance. But after a very short adjustment period, performance commonly improves. Do you have more questions regarding musician’s injuries? Please leave a comment or give us a call. |
Physio Sport Med
Serving all of Oakville in the Uptown / Dundas-Trafalgar Core. Archives
May 2025
Categories |
- Info
- Book Now
-
Team
-
How We Treat
- Sport Medicine Consultation
- Manual - Exercise Physio
- Sport Physiotherapy
- Tissue Injections
- Acupuncture
- Vestibular Physiotherapy
- Osteopathy
- Chiropractic Care
- Concussion Program
- Shockwave Therapy
- Female Pelvic Health
- Male Pelvic Health
- Registered Massage Therapy
- Nutrition Consultation
- On-Field Therapy Coverage
- Custom Orthotics
-
What We Treat
- Sports Injuries
- Low Back Pain
- Osteoarthritis
- Motor Vehicle Accident
- Sprains
- Muscle Strains
- Concussion
- Rotator Cuff
- Tendonitis
- Neck Pain and Headaches
- Hip Pain
- Shoulder Pain
- Elbow, Wrist and Hand Pain
- Foot and Ankle Pain
- Post Surgical Rehabilitation
- Gait and Balance Disorders
- Knee Injuries
- Pelvic Floor Conditions
- Blog
 RSS Feed
RSS Feed