|
And Physiotherapy Can Help!
Have you ever rolled over in bed or looked up quickly and suddenly felt like the room was spinning? You might have thought, “Whoa, am I dizzy, or is the ceiling moving?” If this sounds familiar, you could be experiencing something called Benign Paroxysmal Positional Vertigo — or BPPV for short. It sounds like a mouthful, but don’t worry — it’s a common and treatable condition. And yes, physiotherapy can really help! So, What Is BPPV? Let’s break it down:
In simple terms, BPPV happens when tiny calcium crystals (called otoconia) in your inner ear get loose and end up where they don’t belong. Your inner ear helps with balance, and when these crystals float around in the wrong spot, your brain gets mixed signals about movement — cue the spinning sensation. Common triggers for BPPV include:
The dizziness usually lasts for a few seconds to a minute but can feel very unsettling. How Can We Help? Here’s the good news — BPPV is one of the most treatable forms of vertigo, and our physiotherapists are trained to help you manage it. We use gentle, guided movements called repositioning maneuvers to move those loose crystals back where they belong. The most common technique is called the Epley maneuver — you might also hear about the Semont or Brandt-Daroff exercises, depending on your symptoms. These treatments usually take just a few sessions, and many people feel a huge improvement right away! What Can You Expect at Your Physiotherapy Appointment?
Final Thoughts BPPV can be frustrating, but the solution is often simple and effective. If you’re dealing with dizziness or vertigo, don’t just “wait it out” — book an appointment with our physiotherapist. We’re here to help you get back to feeling steady and confident again! 👉 Feeling dizzy? Don’t let BPPV keep you off balance — book an appointment with David N or Trish today and let’s get you steady on your feet again!
0 Comments
🏀 A Physiotherapy Ode to the 2025 Basketball Playoffs 🏀
1️⃣ The Classic Ankle Sprain AKA: “I landed on someone’s foot” One second you’re going up for the rebound; the next, you’re on the floor clutching your ankle. Welcome to the most frequent basketball injury! Ligaments get stretched or torn, and suddenly that dream of dunking is replaced with the reality of hobbling. How physio helps: We’ll get the swelling down, restore strength and stability, and teach you exercises so your ankle is ready to face the court again — hopefully with fewer landings on unsuspecting feet. 2️⃣ Jumper’s Knee (Patellar Tendinopathy) AKA: “I thought I could still dunk like I was 20” Jumping is fun. Landing repeatedly, not so much. Over time, the tendon that connects your kneecap to your shinbone can become irritated and painful. You might not even notice until stairs start feeling like Everest. How physio helps: Treatment includes targeted strengthening, load management, and manual therapy to calm that cranky tendon — so you can jump (and land) without grimacing. 3️⃣ Rotator Cuff Strain AKA: “I really overcommitted on that half-court pass” Basketball isn’t all about legs — your shoulders get a workout, too. A strained rotator cuff can leave you wincing through jump shots, free throws, and even the celebratory wave to your fans (aka your dog). How physio helps: We’ll assess the injury, work on mobility and strength, and ensure your shoulder is playoff-ready — or at least driveway-shootout-ready. 4️⃣ Jammed Fingers AKA: “Ball meet finger. Finger meet swelling.” Few things are more annoying than a jammed finger. It may seem minor, but left untreated, stiffness and pain can linger longer than your bracket survives the first round. How physio helps: Proper treatment can reduce swelling, restore movement, and get your grip back so you can confidently catch, dribble, and high-five your teammates. Final Thoughts: Play Hard, Recover Smarter Whether you’re a weekend warrior, a rec-league hero, or just shooting hoops for fun, remember this: the NBA players have a whole team of physios keeping them in top form — and you can, too! So as you enjoy the 2025 playoffs (Go Pacers!) Keep an eye on your body. If something starts to ache or swell, don’t just “walk it off” — come see us. We’ll help you stay off the injured list — and maybe even improve your game. 🏀 Call us today to book an appointment — because every player deserves a good support team! 🏀 Shoutout to the Heroes Who Tape Ankles, Save Backs, and Remind Us That Ice Isn’t Just for Cocktails
It’s June in Canada — the month when the sun finally shows up, patios reopen, and… we celebrate National Athletic Therapy Month! While everyone else is planning cottage weekends, we’re tipping our foam rollers to the incredible folks keeping our joints moving and our muscles happy: Certified Athletic Therapists. You might think Athletic Therapists only hang out at sports fields, sprinting in with med kits every time someone pulls a hammy. But let us introduce you to their quieter, less dramatic cousin — the Clinical Athletic Therapist — the unsung hero of recovery rooms, clinics, and rehab spaces across Canada. What Exactly Is an Athletic Therapist? Think of them as the Swiss Army knives of the injury world. Certified by the Canadian Athletic Therapists Association (CATA), these professionals are trained to assess, treat, and rehab all things musculoskeletal — that’s fancy talk for bones, joints, muscles, and tissues that hate stairs after leg day. They use a combination of:
The Clinical Athletic Therapist: Not Just for Pro Athletes Here’s the plot twist: you don’t need to be an Olympian or a professional hockey player to see an Athletic Therapist. In fact, most of their clients are regular humans — office workers with sore necks, parents with aching backs, gym-goers who went a little too hard on leg day, or weekend warriors who believe they can still “go full out” like they did in college. (Spoiler: they can’t.) In a clinic setting, Athletic Therapists focus on getting you back to doing what you love — whether that’s chasing your kids, walking your dog, lifting at the gym, or just being able to sneeze without throwing your back out. Why Their Work Matters (Even If You’re Not Made of Muscle) Musculoskeletal injuries are one of the top reasons Canadians visit healthcare professionals. Clinical Athletic Therapists help people:
Their goal? To get you moving better, faster — ideally with fewer “Oofs” and “Aarghs” every time you stand up. At Physio Sport Med, Carmen is a registered massage therapist, but is also a certified Athletic Therapist. Book now to make use of her many talents.
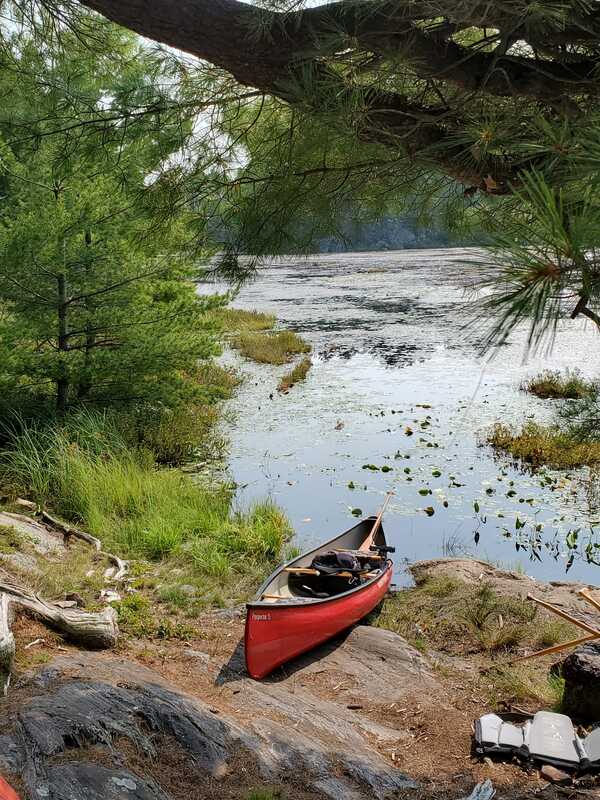
Rotator Cuff Rescue: Paddle With Purpose Paddling may feel effortless at first, but those shoulders will notice after a few lakes. Avoid overuse injuries by switching paddle sides often, keeping your strokes smooth, and engaging your core—not just your arms. A strong core = a happy shoulder. And take breaks! The loons will wait. Portage Without Punishment Portaging is not a race (unless you're my son). Bend at the knees, keep loads balanced, and if your canoe makes you look like a cartoon sandwich, redistribute that gear. A hiking pole or sturdy stick can help on rough trails. And don't forget to stretch those hip flexors afterward—they’ve been doing more work than they signed up for. Tent Time = Stretch Time After a day of adventure, take 5–10 minutes to stretch before crawling into your nylon cocoon. Focus on your back, hips, and hamstrings. Trust me, your spine will thank you in the morning. Enjoy the Trip—And the Recovery Nature’s beautiful—but she’s not gentle. So prep your body, listen to it, and when you return with epic stories and mildly sore glutes, we’ll be here at PSM with open arms, foam rollers, and zero judgment. Happy paddling—and may your blisters be small and your memories big.
Different Demands on Your Body
Running on a treadmill offers a smooth, cushioned surface with consistent conditions. It's ideal during our long Canadian winters, helping runners maintain fitness when roads are icy or trails are snow-covered. But once spring hits and you head outside, you’re suddenly dealing with uneven sidewalks, changing terrain, wind resistance, and hills. These variables engage your muscles and joints in new ways—especially the ankles, knees, and hips. If you've been on a treadmill all winter, your body may not be used to these challenges, making you more prone to overuse injuries like shin splints, IT band syndrome, or Achilles tendinitis. How to Transition Safely This Spring
Spring is a great time to reconnect with nature and your fitness goals. With a mindful transition, you can enjoy the season injury-free. If you have questions about your running form or want help preventing injuries, our clinic is here to support your spring comeback! Enhancing Recovery: The Benefits of Adding Massage Therapy to Physiotherapy or Chiropractic Care5/5/2025 Incorporating massage therapy into a physiotherapy or chiropractic treatment plan can significantly enhance overall recovery and well-being. While physiotherapists and chiropractors focus on structural alignment, mobility, and function, massage therapy complements these goals by targeting soft tissues to relieve muscle tension, improve circulation, and reduce stress. Massage therapy promotes faster healing by increasing blood flow to affected areas, which helps deliver oxygen and nutrients essential for tissue repair. This can be especially beneficial after injury or surgery, where reducing inflammation and enhancing flexibility are key to regaining function. Additionally, massage can help prepare muscles for manual adjustments and improve range of motion. Another major benefit is pain reduction. Therapeutic massage stimulates the release of endorphins—natural painkillers—helping patients manage chronic or acute discomfort more effectively without relying solely on medication. Furthermore, the relaxing nature of massage therapy contributes to reduced anxiety and improved sleep, both of which are critical for long-term recovery and physical performance. When combined with physiotherapy or chiropractic care, massage therapy offers a holistic approach that addresses both the structural and muscular components of pain and dysfunction, leading to more comprehensive and lasting results. Meet our team  Michael Burrow Michael graduate in 2018 earning the Sports Outreach Specialization Award. His background in competitive sport allows him to understand and treat common injuries found in the athletic community. He incorporated Functional Range Conditioning and Functional Range Systems into his treatments to maximize recovery. Recently, Michael started offering Fascial Stretch Therapy. FUN FACT: Michael played Junior A lacrosse for Mimico, so he is able to understand the demands and pressures on amateur athletes.  Liia Wu Proficient in deep tissue, sports and relaxation massage, Liia integrates cupping therapy and gua sha therapy into the treatments. Currently enrolled in the Acupuncture program at CCTCM, she is committed to expanding her healthcare practice. Yifan believes that integrating acupuncture and acupoint massage will significantly enhance her ability to alleviate clients' pain and improve their overall well-being. FUN FACT: Yifan-Liia has decades of experience playing the violin, brings a unique perspective to her practice.  Carmen Chan Carmen’s massage therapy practice is shaped by over a decade of experience as a Certified Athletic Therapist. She is passionate about working with all athletes and has worked extensively in hockey, volleyball and ultimate frisbee. Carmen strongly believes that a successful treatment plan requires collaboration between the practitioner and client. FUN FACT: Carmen is learning American Sign Language and has been the medical support for the Deaf Olympics.
So, what makes Fascial Stretch Therapy stand out? Let’s break down its key benefits: 1. Improved Flexibility and Mobility Unlike traditional stretching, which focuses on isolated muscles, FST works on entire muscle groups and their connective tissue. This helps increase range of motion more effectively and sustainably. Whether you're an athlete looking to enhance performance or someone who just wants to move with more ease, FST can help you move better and feel better. 2. Reduced Pain and Tension Chronic tension in the fascia can contribute to joint pain, back discomfort, and muscle tightness. FST gently targets these areas, releasing restrictions and reducing pressure on pain-sensitive structures. Many clients report a significant reduction in discomfort after just a few sessions. 3. Enhanced Athletic Performance By improving joint range and muscle efficiency, FST can help athletes generate more power and reduce the risk of injury. It also aids in faster recovery by promoting circulation and reducing muscle soreness after intense workouts. 4. Stress Relief and Relaxation FST sessions are often described as calming and restorative. The gentle, rhythmic movements not only stretch the body but also calm the nervous system, making it a great tool for managing stress and promoting overall well-being. 5. Posture Correction Poor posture often stems from imbalances in the fascia. FST helps realign the body by loosening tight areas and strengthening weak ones, leading to better posture and less strain on your body throughout the day. Whether you're rehabbing from an injury, enhancing your athletic routine, or simply seeking better body balance, Fascial Stretch Therapy is a versatile, effective approach to total-body wellness. There’s just something about my backyard that makes me happy. Whether it’s a summer barbecue, a family campfire, or simply enjoying my morning coffee in the fresh air, it’s my favorite spot to relax. But here’s the thing—those who know me will tell you, I’m not much of a gardener.
That said, this is the year that’s going to change. I’m determined to create the backyard I’ve always dreamed of, and it all started just yesterday. Armed with clippers and a yard waste bag, I finally tackled the straggly mess that winter left behind. I admired the little flowers poking through and smiled at the green buds on my berry bushes… right before a thorn made itself known in my thumb! And as I bent down to my toes for what felt like the 20th time, I had an important reminder—gardening is hard work on the body. So, for anyone else dreaming of a better backyard this year, here are five tips to help you garden without the aches and pains:
What is Osteopathic Manipulation Treatment (OMT)? OMT involves the use of the practitioner’s hands to examine and treat the patient’s body. It considers the body as an interconnected system rather than treating individual symptoms in isolation. It emphasizes the body’s natural ability to heal itself. How does OMT work? The principle behind OMT is that the body’s structure and function are closely intertwined. If the structure (like bones, muscles, and joints) is restricted or stuck, if can affect the vascular and nerve to the whole body’s function. Osteopathic practitioners use their hands to feel for abnormalities of your joints, muscles and other tissues. The then use a variety of techniques, such as stretching, gentle pressure and resistance, to help alleviate pain, restore function and promote overall health. What Conditions Can OMT Treat? OMT is used to treat a wide range of conditions. It can help with pain relief, such as back pain, neck pain and headaches. It’s also used for other issues like asthma, sinus disorders, digestion issues and menstrual pain. Beyond treating specific conditions, OMT helps improve overall wellness and mobility. Is OMT Safe? Yes, when performed by a trained osteopathic practitioner, OMT is safe. It’s a non-invasive treatment and can be an alternative to medication and surgery for certain conditions. As with any medical treatment, it’s important to discuss your health history with the practitioner to ensure OMT is appropriate for you. Is OMT covered by extended healthcare insurance? Every insurance policy is different, so we always encourage people to check their plan. However, often Osteopathy is covered in the paramedical section of extended healthcare insurance. Do you need a doctor’s referral? No, you are welcome to have osteopathy treatment without a referral. Osteopaths are considered primary practitioners, which means it is safe to attend without a referral. Although rare, some insurance companies may ask for you to have a referral.
Don't worry; getting physically ready for outdoor cycling in the spring is all about gradual preparation and reintroducing your body to the rhythm of cycling. Here’s how you can safely and effectively get back into the saddle after a winter break.
1. Start Slow and Build Gradually It can be tempting to jump right into long rides or high intensity cycling sessions, but your body needs time to adjust. Riding outside places different and often higher demands on your muscular and cardiovascular systems. Start with shorter, easy rides to get your legs back under you. Initially flatter rides are better. The Canadian Academy of Sport and Exercise Medicine recommends a 10% increase in workload per week. Workload consists of volume and intensity. So, if you are adding a hilly route, decrease your watts, speed or length of time accordingly 2. Stretching and Flexibility Cycling places a lot of demand on your legs, hips, and lower back, so it's essential to work on mobility before hitting the road. If you have used a stationary, or no bike, during the winter make sure that you have the spinal and hip mobility to rest comfortably in your fit. Consider adding dynamic stretching into your pre-ride routine. Leg swings, walking lunges, or even some gentle hip rotations can help loosen up your muscles before setting off. Long static stretching should wait until after the ride is over but can be easier to do when the muscles are warm. 3. Focus on Core Strength Cycling is not just about your legs; your core plays a crucial role in maintaining posture, balance, and control while on the bike. A strong core will make your rides more comfortable and reduce the risk of back or neck strain. If you’ve taken the winter off from cycling, you might find that your core has weakened, so it's time to include some core-strengthening exercises in your routine. Dead bugs and Mountain climbers are great basic core exercises for cyclists. Remember to keep the back and core stabilized and still during hip flexion. 4. Listen to Your Body As you transition back to cycling outdoors, be mindful of how your body is feeling. If you experience any pain or discomfort, don’t push through it. Take rest days when needed, and allow your body to recover between rides. Cycling should be fun, not a cause of injury or frustration. A general rule of thumb is that if pain is not resolving after 3 days you should seek advice from a physiotherapist, chiropractor or physician. 5. Gear Up for the Weather Spring can be unpredictable, with some days being warm and sunny while others bring cooler temperatures or rain. Be prepared by layering your clothing to stay comfortable. Opt for moisture-wicking base layers that will keep sweat off your skin, and bring a lightweight jacket in case the weather turns chilly or rainy. Additionally, don’t forget about safety gear. A well-fitting helmet, proper cycling gloves, and sunglasses for sun and wind protection are all essential parts of your outdoor cycling kit. 6. Tuning Up Your Bike It goes without saying that you bike might need a little attention as well. Transition time is a great time to check that everything is in working order. Make sure your tires are properly inflated, the chain is clean and lubricated, and the brakes are functioning smoothly. A bike that’s in good working condition will make your rides safer and more enjoyable. The roads are still dirty, and the weather is still cool, so take the time now to do the prep work. We will be back on the open roads in no time. Can’t wait to see you out there.
Erica will complete a thorough history, physical examination and report of findings that will allow you and encourage you to ask questions, listen to your concerns and involve you in care!
Treatment depends on your goals, clinical expertise and best available evidence! If you are not comfortable with a specific treatment or specifically spinal or extremity manipulation, then it does not need to be done! As you can see, there are plenty of other options that can help you feel your best. As a chiropractor, Erica prides herself in continual education to be able to offer you different styles of care to suit everyone’s individual needs. If you are wondering if seeing a chiropractor is right for you and you are hesitant, feel free to book a consultation to discuss! Physio Sport Med of Oakville Trish Hayton in Thailand Traveling with a National Team is an exhilarating and rewarding experience, one that blends hard work, perseverance, and a bit of luck. Many people ask me how I ended up in this role and what it entails. Here’s a glimpse into the journey and what I do on the road as a sports physiotherapist. The first step to getting here was qualifying. After graduating as a physiotherapist, I entered the Sports Physiotherapy education system, which involves gaining experience, completing a mentorship, and passing practical exams. Upon earning the Diploma of Sports Physiotherapy, I was qualified to work at international competitions. During the process, I built my experience, starting with local rugby, lacrosse, and hockey teams, before moving to provincial-level events and eventually the Canadian Games. However, the major leap in my career came when I left a clinic job I loved to work at the Pan and Parapan Am Games, which opened the door to international competitions.  Once qualified, my job begins long before we take off. Preparation is key. I pack a kit that includes everything needed for therapy, taping, first aid, and general health care. Over the years, I've perfected this kit, but there's always something new that pops up. For example, this trip’s unexpected item was hair elastics. As teams often don't travel with a nutritionist, I’m also responsible for gathering between game fuel such as energy bars, apple sauces, and electrolytes. In addition to packing, I research specific health risks at our destination. For instance, when we traveled to Thailand, I ensured all athletes and staff were up to date on necessary vaccines and provided education on local health concerns like water and mosquito-borne viruses. I also prepared heat strategies, as the temperatures in Bangkok were expected to reach 34-37°C. This is a drastic change for a bunch of Canadian travelling in March. Once we arrive, the work truly begins. On the ground, I’m responsible for daily treatments, first aid, and pre-game care. As the only medical support traveling with the team, I’ve had to address everything from pneumonia to food poisoning. Sports physiotherapists are often called upon to play multiple roles, including makeshift strength and conditioning coach, brace repair technician, and even mental therapist. Thankfully, I’m supported by a team of experts back home who assist with medical advice. Although there are challenges, I would not trade travelling with these teams for anything. Through supporting our amateur teams, I get to see the world while striving for my ultimate goal – being part of team Canada at the Olympics. Trish Hayton is a Physiotherapist and Partner - Owner at Physio Sport Med of Oakville.
March Break is a time to relax, explore, and recharge, but it’s also a time when injuries can easily happen if you’re not careful. Whether you’re heading to a sunny beach, a snowy mountain, or an exciting city, here are some tips to help keep you safe and injury-free during your travels.
1. Pack Smart Packing light and correctly can prevent strain on your body. Overpacked bags can lead to back and shoulder injuries, especially if you’re carrying them for long distances. Opt for a backpack with padded straps and a waist belt to distribute the weight evenly. Roll clothes instead of folding them to save space and reduce stress on your body. Be careful when pulling a packed suitcase behind you. This is a vulnerable position for the shoulder and a small snag could result in pain. 2. Keep moving Long flights or road trips can take a toll on your body. Picking an aisle seat so that you can get up and stretch a little easier can be helpful. If you are driving, stopping every 2-3 hours is recommended to stretch your back and legs. Fatigue can also lead to accidents, so be sure to get plenty of rest and avoid pushing your body too hard. 3. Be Mindful of Your Surroundings When traveling in unfamiliar places, keep an eye on the terrain. Whether you're walking on slippery sidewalks or hiking in the mountains, watch where you step. Be cautious on unfamiliar stairs or curbs, and wear comfortable, non-slip footwear. 4. Know Your Limits It’s tempting to dive into all the fun activities available during March Break, but know your limits. If you’re trying something new, like snowboarding or rock climbing, start with a beginner course or lesson. Pushing yourself too hard can lead to injuries that could ruin the rest of your trip. 5. Warm Up Before Activities If you’re planning on skiing, hiking, or any physical activity, take a few minutes to stretch and warm up your muscles. This simple step can help prevent strains and sprains. Even if you’re just walking around a new city, stretching your legs can make a big difference. With a little preparation and attention, you can enjoy all the excitement of March Break without the setbacks of an injury. Stay safe and have fun! At Physio Sport Med, we believe in giving our patients the best possible care – which is why we integrate osteopathy and physiotherapy into personalized treatment plans. While both disciplines aim to restore health and mobility, they work in unique yet complementary ways. Here’s how combining them can help you recover faster and stay stronger for longer.
The Power of Collaboration - Whole-Body Healing Meets Targeted Rehabilitation
Together: This dual approach tackles both the root cause (e.g., joint restrictions, fascial tension) and the symptoms (pain, weakness) of your condition. Pain Relief + Functional Recovery
Together: You get dual-action pain relief and a faster path to moving freely again. Prevention for Long-Term Wellness
Together: You’ll not only recover but also stay active, healthy, and pain-free long after treatment. Who Benefits Most from Combined Care? This approach is ideal for:
Why Choose Our Integrated Care?
Since 2014, Canada has had the honour of hosing the Invictus Games two times. In 2017, Toronto hosted a summer version of the games. At that time, we welcomed 539 competitors from 17 nations, including Romania, Iraq and Ukraine, who were competing in their first games. There were 8 days of fierce competition spread over 12 adaptive sports. Due to her work at the Pan/Parapam Am Games, Trish became a lead volunteer for this event. Even though her resume has gotten much longer, Trish still states, “to this day it is my favourite multigame experience, and it is due to the spirit of athletes celebrating rehab, recovery and success.”
In February, British Columbia hosted the first winter version of the Invictus Games, including 500+ athletes, 23 nations and 11 winter sports held across Vancouver and Whistler. We are so proud that James was selected as a sponsored medical practitioner and spent 8 days in Vancouver assisting with the medical treatment of the athletes. Luckily, he wasn’t too busy. But he admits that his favourite moments included watching the gold medal Wheelchair rugby game between United Kingdom and France and meeting Prince Harry. It was also his first trip to British Columbia; he discovered the beauty of our west coast, and hopes to return for some camping and hiking. The next Invictus Games will be held in Birmingham, UK in summer of 2027. Who knows, maybe Trish will head back to her Commonwealth stomping ground…
1. Eat Heart-Healthy Foods Heart health thrives on a nutritious diet. Embrace heart-healthy foods like leafy greens, berries, nuts, and fish rich in omega-3 fatty acids, such as salmon. Foods that are high in fiber and low in unhealthy fats can help maintain healthy cholesterol levels and reduce the risk of heart disease. 2. Exercise Regularly Regular exercise is one of the best things you can do to improve heart health. It strengthens the heart muscle, improves circulation, and helps maintain a healthy weight. Aim for at least 30 minutes of moderate activity a day —whether it’s walking, swimming, or dancing to your favorite love songs. 3. Manage Stress The stress of everyday life can take a toll on your heart. Take a step back to manage stress in healthy ways. Meditation, deep breathing exercises, or simply spending quality time with loved ones can help lower stress levels and promote heart health. 4. Get Regular Check-Ups Lastly, never underestimate the power of preventive care. Regular check-ups with your doctor help monitor blood pressure, cholesterol, and other heart health indicators. Taking care of your heart is the ultimate act of love—both for yourself and for those you care about. So, this February, let’s commit to living heart-healthy lives long after the chocolates have been eaten and the flowers have wilted. What is a Sports Medicine Specialist and when should I see them.
Sports medicine physicians play a crucial role in maintaining and enhancing the health and performance of athletes in Ontario. They are medical professionals with specialized knowledge in preventing, diagnosing, and treating injuries related to sports and physical activity. These physicians are trained to handle a wide range of conditions, from acute injuries such as fractures and sprains to chronic issues like tendinitis, osteoarthritis and overuse injuries. Sports medicine physicians work closely with athletes at all levels, from recreational participants to elite professionals. Anyone that is trying to maintain an active lifestyle can be successfully treated by a sports medicine specialist. Our sports medicine physicians collaborate with our other healthcare providers, including physiotherapy, massage therapy, athletic therapy, osteopath, chiropractor and dietitian. Together they determine the best approach and most efficient way of getting you back to the life you enjoy. They also educate athletes on proper nutrition, hydration, and injury recovery strategies to support long-term health and performance. Do you need a referral to see a Sports Medicine Physician? For most issues we do ask that you get a referral from your family physician. This ensures that the appropriate investigations have already been completed, and you can get the most from your visit. It also keeps your family physician in the circle of care so that your healthcare treatment is well coordinated. But we do recognize that in today’s healthcare environment getting into see a family physician can be challenging. And when you have hurt yourself, it is important to get rapid and expert care as soon as possible so that you get back to the game as soon as possible. That is why we have introduced our RAPID ACCESS PROGRAM. If you have injured a bone, joint or muscle within the last 10 days, you are bumped to the front of the line and can see one of our expert specialists as soon as possible. No referral or investigations necessary. The team at Physio Sport Med has grown again. Two amazing massage therapists have joined Michael on our team. This means that we are happy to offer massage therapy 6 days a week for your convenience and care. Liia is an experienced musician that brings a different perspective to her treatments. She recognizes that musicians share many of the same injury concepts as elite athletes including overuse and repetitive strain injuries. Liia also adds cupping therapy and Gua sha therapy into her treatments. Dedicated to education, she is adding to her skills but studying Acupuncture and Acupressure.
Carmen is a certified athletic therapist and registered massage therapist. She has treated a variety of athletes, from recreational to professional to industrial. As part of medical teams, Carmen has attended many high performance events including Pan American Games, Deaflympics and Canada Games. She is passionate about working with all athletes and has worked extensively in hockey, volleyball and ultimate frisbee. She uses Swedish massage techniques accompanied with trigger point therapy, fascial release and craniosacral techniques.  Sprained ankle? Pulled Muscle? Blown Out Knee? We know that getting rapid and expert care after a sports injury can be difficult and frustrating in today’s medical system. That is why we are introducing out Acute Care Rapid Access Program.
If you have any musculoskeletal injury that has happened within the last 10 days, you qualify. This means that any new injury (or re-injury) of a muscle, bone or joint will allow you to jump the waiting list for our physiotherapists and sports medicine specialist physicians as we know that immediate and high-quality care not only gets you stronger and better faster, but results in better healing and reduces the chance of future injury and arthritis. We do not need a referral from your family doctor, and we do not need X-rays or Ultrasound. Call the clinic directly, state that you have a new injury, and the process will get started. Please note that at times your insurance will ask for a referral for physiotherapy or chiropractor services. If you see our physicians, they can help with this. We look forward to working with you and keeping Oakville active and healthy. Pelvic floor issue in men could be as a result of surgery, infection, traumatic events, being overweight, repeated heavy lifting and poor posture. Some of the most common symptoms include
Some of the common conditions men may experience include:
How can Pelvic Physiotherapy Help We can provide you with detailed pelvic floor examination, offer manual therapy to assess tone in pelvic floor muscles, mobilize scar tissue, teach you to either relax or strengthen your pelvic floor and strategies to manage your symptoms. At Physio Sport Med Pelvic Health is one of our specialties. Call for an appointment. 905 257-3456.
At Physio Sport Med of Oakville quality personalized care is our primary focus. We encourage our practitioners to continue post graduate education. This ensures that our clients get the most effective care based on current research and best practices. To reflect this value, we will be introducing tiered pricing for our physiotherapy clients starting on Monday September 23rd. The tiers will be defined as follows:
Associate Physiotherapists who are licensed to practice in physiotherapy in Ontario. These therapists are continuing to participate in post graduate studies and develop their specialty. Our current associates are: Christine, David, George, Ansu (for orthopedic clients) Senior Associate Therapists have achieved highest level of education/certification in a discipline including Orthopedic Mobilizations and Manipulations (FCAMPT), McKenzie Mechanical Diagnosis and Treatment, Sports Physiotherapy (Diploma Level), Pelvic Physiotherapy (Level 3) or Canadian Physiotherapy Association. Our current senior associates are: Paul, James, Ansu (for pelvic physiotherapy clients) Partner Therapists have achieved at least one of these education levels and have demonstrated leadership in the company or the therapist has achieved 2 or more of the qualifications above in different specialties. Our current partner therapists are: Trish Effective September 23 the following rates will apply.
 Are you ready to take your golf game to the next level? We’re here to introduce you to a game-changing approach that could revolutionize your performance on the course: Osteopathic Manipulative Treatment (OMT). What is OMT? OMT is a holistic approach designed to enhance your golfing performance by improving mobility, reducing muscle tension, and promoting overall physical well-being. With golf being a sport that demands precision, flexibility, and power, OMT could be the answer to more consistency in your game. How Can OMT Benefit Golfers? Improved Hip Mobility Studies have shown that OMT can enhance hip range of motion and reduce pain, allowing you to achieve a better swing rotation and follow-through for that powerful drive down the fairway. This is particularly beneficial for golfers who struggle with maintaining posture and early extension. Systematic reviews have highlighted the effectiveness of manual therapies in improving hip joint function, muscle strength, and overall mobility. Enhanced Thoracic Mobility OMT techniques such as articulation mobilization and myofascial release can improve thoracic spine mobility, leading to better posture and a more consistent swing, while reducing the risk of injuries. This is necessary for golfers who struggle with coming over the top and tend to slice or hook the ball. Enhanced thoracic mobility can lead to a more consistent and powerful swing. Reduced Muscle Tension OMT is effective in relaxing tight muscles and improving circulation, promoting faster recovery and better performance on the course. These methods help maintain muscle balance and flexibility, which are critical for the repetitive and precise movements required in golf for all 18 holes. Techniques like myofascial release and muscle energy work to relax tight muscles and improve circulation, enhancing overall performance. Clinical Evidence Supporting OMT Numerous studies have underscored the efficacy of OMT in improving physical function and mobility. For example, research published in prestigious journals like BMJ Open and PLOS ONE has highlighted the wide-ranging benefits of OMT for various clinical conditions, emphasizing its role in enhancing mobility and overall physical performance . Conclusion Osteopathic Manipulative Treatment offers a comprehensive approach to improving golfing performance through enhanced mobility and reduced muscle tension. By incorporating OMT into your training regimen, you can achieve greater flexibility, power, and consistency in your swings, while promoting long-term physical health. Embrace the benefits of OMT and take your golf game to new heights. By integrating the benefits of OMT into your golfing routine, you’re not only investing in better performance but also in your overall physical health. Ming Su, RMT., M.OMSc The Canadian Academy of Manipulative Physiotherapy (FCAMPT) recently published some great Q&A pages on Physiotherapy generically, and on some specific treatment topics. Check them out!
Check out our FCAMPT accredited physiotherapists at Physio Sport Med of Oakville and make an appointment to get the help you need! NHL, NBA and MLB are on TV. I am inspired by the new NIKE “Can’t stop us ad.” (If you haven’t seen it, follow this link: https://www.youtube.com/watch?v=WA4dDs0T7sM). Gyms across the province have opened. And my family is returning to the ice and warming up for fall field lacrosse. Sports are back. They are different, but they are back.
There are few things to keep in mind as we return to the playing fields, courts, and workout centers.
We have now been seeing patients in the clinic for two full months and while things are a little different, providing first class care remains the same. During the shut down we took this time as an opportunity to revamp our internal software system. This dramatically improved our ability to take online bookings for many practitioners. You can start by going here to see all your options. We also started providing "virtual appointments", which we continue to provide as an option for those patients who feel more comfortable starting with an online visit.  When you do come to the clinic you will see that things are a little different. At Physio Sport Med of Oakville we follow the Ontario Provincial guidelines along with the guidelines specified by the various colleges that regulate our practitioners. This targets the safety of our patients, practitioners and staff. We take it seriously. Here's what you should expect at your next visit.
While Ontario has done very well so far to bring Covid numbers down, we continue to recognize the need to be vigilant to help avoid local outbreaks and the feared second wave. Please help us in this endeavor when you come to visit. As you get back into your regular exercise routine rest assured that we are here to help with any issues or injuries that you encounter. Thank you very much for your continued business! |
Physio Sport Med
Serving all of Oakville in the Uptown / Dundas-Trafalgar Core. Archives
May 2025
Categories |
- Info
- Book Now
-
Team
-
How We Treat
- Sport Medicine Consultation
- Manual - Exercise Physio
- Sport Physiotherapy
- Tissue Injections
- Acupuncture
- Vestibular Physiotherapy
- Osteopathy
- Chiropractic Care
- Concussion Program
- Shockwave Therapy
- Female Pelvic Health
- Male Pelvic Health
- Registered Massage Therapy
- Nutrition Consultation
- On-Field Therapy Coverage
- Custom Orthotics
-
What We Treat
- Sports Injuries
- Low Back Pain
- Osteoarthritis
- Motor Vehicle Accident
- Sprains
- Muscle Strains
- Concussion
- Rotator Cuff
- Tendonitis
- Neck Pain and Headaches
- Hip Pain
- Shoulder Pain
- Elbow, Wrist and Hand Pain
- Foot and Ankle Pain
- Post Surgical Rehabilitation
- Gait and Balance Disorders
- Knee Injuries
- Pelvic Floor Conditions
- Blog



















 RSS Feed
RSS Feed